Cardiac arrhythmias should not be overlooked as a probable cause of nocturnal bedwetting
When a usually docile individual has enuresis nocturna, researchers present a persuasive, evidence-based case for broadening the diagnostic workup to include cardiac arrhythmias (involuntary urination during sleep).
Recommendations for how to treat people with heart rhythm problems have been written up in the journal of the three groups. The Heart Rhythm journal is the official journal of the three groups: Heart Rhythm.
When a normally healthy person develops nocturnal enuresis, treating doctors usually rule out urinary tract infections, anatomic anomalies, emotional disorders, epilepsy, sleep apnea, and the side effects of diuretic or sedative drugs.
Involuntary urination during sleep can be an indication of certain potentially fatal cardiac arrhythmias, but it is rarely recognized in the diagnostic process.
The death of a 23-year-old woman who had two isolated bedwetting episodes but no other symptoms of long QT syndrome type 2 motivated researchers to look into the current practices used by clinicians who are likely to encounter patients with unexplained enuresis.
They ran an anonymous internet-based survey in which doctors were asked to choose which diagnostic tests they would order for a patient with unexplained bedwetting and no other symptoms.
102 pediatricians, 73 family physicians, 57 internal medicine specialists, 35 residents, 37 interns, and 42 advanced medical students were among the 346 respondents. There were 114 senior physicians with more than three years of experience among the group.
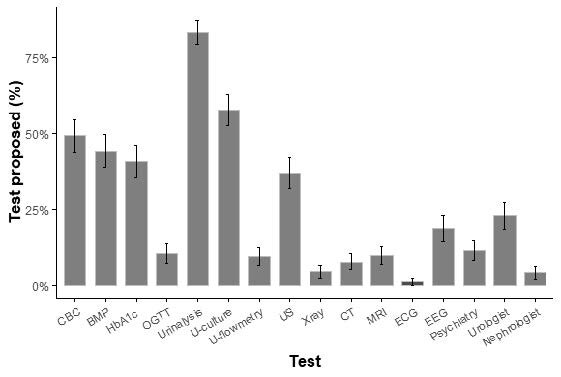
Following episodes of enuresis, the majority of survey respondents claimed they would undertake urinalysis and kidney ultrasonography to look for an underlying urinary condition.
Testing for diabetes and irregularities in urine flow were other popular choices. While 19% recommended an encephalogram, indicating that they thought nocturnal epileptic seizures could be the cause, only 1% thought an electrocardiogram was necessary.
As evidenced by this result, arrhythmic seizures are almost never investigated in the differential diagnosis of unexplained enuresis.
“We are both surprised and concerned by the lack of awareness among primary physicians about the possibility of nocturnal arrhythmogenic seizures caused by long QT syndrome,” said lead investigator Sami Viskin, MD, of the Sourasky Tel Aviv Medical Center and Tel-Aviv University’s Sackler School of Medicine.
“The disease, which can be fatal if it isn’t diagnosed or treated, is easy to spot with an ECG and responds well to treatment.”
The medical profession recognizes arrhythmias as a major cause of daytime syncope, and the ECG is a critical tool for diagnosing them. It’s critical to promote awareness that the same rhythms that produce syncope in the “awake patient” can also cause nocturnal seizures when sleeping.
If no one sees the seizures at night, inexplicable bedwetting may be the only thing to show that this was a big event.
Dr. Viskin explained that in most cases of enuresis, the underlying diagnosis is not arrhythmic syncope, especially in young patients. However, because “an electrocardiogram is a cheap and quick test that is important for catching potentially fatal conditions that can be treated,” it is important to look into this option, even if the events are very rare.
“Every medical appointment should include a question regarding a family history of unexpected death,” Dr. Viskin noted. Failure to acknowledge a cancerous family history can have serious consequences: Their patient had a family history of sudden death, as well as a genetic risk.
In an accompanying editorial, Dr. Patrina H.Y. Caldwell, FRACP, Ph.D., and Professor Jonathan R. Skinner, MBChB, MRCP (UK), FRACP, MD, FHRS, both of Sydney Children’s Hospital (Randwick and Westmead, Australia), agreed in an accompanying editorial that taking a family history for early death, in combination with an electrocardiogram, is recommended as a quick, cheap, widely available, and effective way to prevent it.